Practical Tips for Diversity, Equity, and Inclusion in Bariatric Patient Population SPHM and Care
Obesity rates continue to climb in the United States. With them grows the need for updated bariatric population safe patient handling and mobility (SPHM) practices, mindsets, and care.
Inherent to this conversation is the matter of diversity, equity, and inclusion (DEI) – that is, offering fair treatment, opportunities, resources, support, and respect to all patients, regardless of differences including weight.
Below are guidelines from Manon LaBreche for identifying opportunities in your healthcare organization for more equitable bariatric population care, with a focus on SPHM. Beyond offering bariatric patients the treatment and care they deserve, these insights often create easier and safer conditions for healthcare staff. Labreche is a Physical Therapist, Certified Ergonomic Assessment Specialist (level 2), Certified Health Coach, and a Certified Posture Exercise Professional. For the past 23 years she has managed the Injury Prevention Program at Tampa General Hospital, which features a robust SPHM program including a patient handling team.
Of note: Bariatric patients are generally defined as any patient having a body mass index (BMI) equal to or greater than 30. Obesity Class 1 describes patients with BMIs of 30 to 34.9, Class 2 as 35 to 39.9, and Class 3 as 40 and above[1].
THE DIFFERENCE BETWEEN EQUALITY AND EQUITY
Before delving into bariatric patient care opportunities in your organization, a quick visual to help differentiate between equality and equity:

In the image above, equality is represented on the left. It’s the act of giving each person the same resource and hoping they reach their goals.
Equity is on the right. It’s the more intentional practice of offering customized resources to ensure that each person has the opportunity to reach their goals.
Bariatric patients frequently report feeling discriminated against or treated with disrespect by physicians and other personnel; their feedback commonly points to healthcare systems and providers who stop short of equity. Keep this subtle but critical difference in mind as you consider improved practices for bariatric patients.
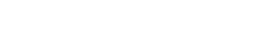
ASSESSING BARIATRIC MOBILITY BARRIERS
The medical consequences of limited patient mobility are well-documented, with implications for every system of the body. Immobility can also contribute to prolonged hospital stays, added healthcare costs, discharge planning challenges, and staff burnout and injury.
Still, bariatric patients are often repositioned and moved less frequently than their non-bariatric counterparts. The reasons are many and are real. There’s a good chance they occur in your healthcare setting:
- Lack of necessary equipment
- Lack of training
- Lack of resources
- Fear of injury
- Environmental barriers
- Lack of standard processes and protocols
- Patient drivers: Fear, anxiety, depression, motivation
These barriers can be daunting. The good news: They can also be overcome. Below, we offer Labreche’s expert insights for overcoming two of them: Lack of necessary equipment and lack of processes and protocol.
SOURCING RIGHT-FIT EQUIPMENT
The right equipment is key to improving mobility and thereby outcomes and lived experiences among bariatric populations. However, Rome wasn’t built in day; nor are full suites of bariatric equipment typically assembled overnight! Over more than twenty years, Tampa General Hospital incorporated the following bariatric equipment and supplies into their larger inventory and practices. Individually and combined, they increase bariatric patient mobility, advance patient goals, decrease staff injury, and make bariatric patient SPHM and care significantly easier, more equitable, and more standardized:
- Air-assisted technology – integral to patient repositioning, turning, and boosting required for linen changes, dressing changes, cleanings, procedures, and routine repositioning.
- Repositioning sheets – same as above. These are particularly helpful when combined with permanently-mounted ceiling lifts.
- Permanently-mounted ceiling lifts – these are superior to portable ceiling lifts, which often limit overhead room, among other barriers.
- Full-length absorbent pads
- Floor lifts
- Bariatric limb slings
- Tilt-bed technology – this technology is ideal for early and frequent weight bearing activities, as it minimizes the risk of team member injury. Especially helpful if the bariatric patient struggles with transitioning from supine to sit (a strenuous activity that commonly exhausts bariatric patients prior to physical therapy).
- Walking slings
- Motorized bariatric stretchers
- Bariatric wheelchairs
- Bariatric treatment tables
- Bariatric commodes and walkers
- Bariatric gowns, wedges, and blood pressure cuffs
- Bariatric seating
Start simple: Consider the greatest barriers to SPHM among your bariatric patients. Which equipment could alleviate those hurdles? Which are most in reach? Bariatric gowns and seating alone can make healthcare settings more accessible and comfortable for patients while alleviating staff challenges, too.
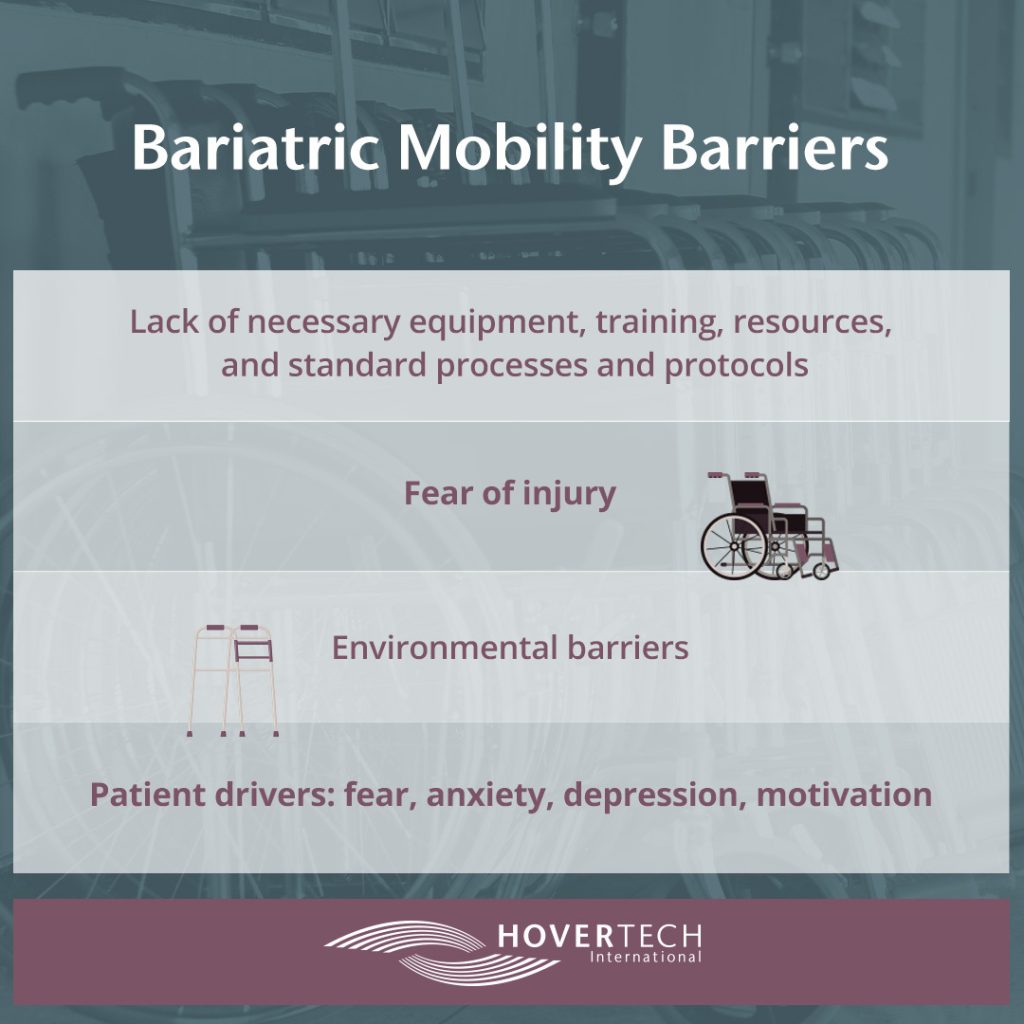
ESTABLISHING PROCESSES AND PROCOTOLS
Protocol shifts within a healthcare facility can also go a long way toward ensuring equity for the bariatric patient population. When considering protocols and processes, it’s important to consider their long-term sustainability. We encourage kicking off with changes that are most urgent and/or most attainable. This bodes well for success, which increases the likelihood of added and expanded processes and protocols moving forward.
A few examples of bariatric patient-minded processes and protocols successfully developed by healthcare facilities including Tampa General Hospital:
Standardized bariatric equipment availability and tracking. In years past, Tampa General Hospital struggled to locate bariatric equipment. This was remedied when the healthcare system’s Epic HER software was expanded to include tags for all bariatric items, making them easily searchable. The portal also includes product information such as weight capacity, tip sheets, training videos, and ordering details.
CareComm or similar ER protocol. Instead of calling the hospital’s bed department upon admission of a bariatric patient, Tampa General Hospital’s emergency department calls CareComm – a department that strives to place the right patient in the right room and monitors related data analytics. This is especially helpful when trying to place a bariatric patient in a room with a ceiling lift upon admission.
Bed transportation protocol. Clear policies exist to minimize bed transportation for all patients regardless of their size. According to Tampa General Hospital’s protocol, patients can be transported in beds only if they meet certain criteria. When this occurs among bariatric patients, the bed must be motorized.
Equipment rentals. If no budget exists for necessary bariatric items like beds, tilt beds, and wheelchairs, consider a standardized process that allows staff to rent them as needed.
Renovation and new construction standards. Over two decades, Tampa General Hospital has developed prerequisites for renovations and new construction, including full room systems featuring XY ceiling lift tracks and permanently-mounted ceiling lifts in each room (motors are stored in an upper cabinet when not in use).
These are just a few of the many opportunities that exist within most healthcare facilities to improve bariatric patient population equity and care. For a more in-depth talk and to earn one free contact hour, listen to the full on-demand webinar.
[1] https://www.pennmedicine.org/updates/blogs/metabolic-and-bariatric-surgery-blog/2019/april/what-does-bariatric-mean#:~:text=A%20person%20is%20classified%20as,weight%20in%20relation%20to%20height.