Creating Safe, Supportive Perioperative Settings for Patients with Bariatric Disease
Class III obesity- a bariatric disease- is on the rise. The perioperative setting needs to assess and develop a plan to adequately support bariatric patients. Read on for helpful tips for your surgical setting, and listen to the full on-demand webinar to earn one contact hour.
Class III obesity, previously known as morbid obesity, is characterized by a body mass index (BMI) of 40 or higher and the presence of obesity-related health conditions.
Language shifts around Class III obesity are part of a larger push to dispel false and problematic stigmas– stigmas that can and do diminish bariatric patient quality of care. Patients with high BMI have been known to avoid preventative screenings and even necessary treatment for fear of healthcare provider biases and other oversights and insensitivities.
It is critical, then, to not only address attitudes of physicians and staff, but to assess and ensure a perioperative healthcare setting’s ability to move, accommodate, and comprehensively treat all patients equitably – regardless of size. Put another way, perioperative team members need to identify patients at risk for BMI-related injuries and discomfort, then develop customized plans to keep them safe and maintain their dignity before, during, and after surgical procedures.
Luckily, there are tools. Below are high-level guidelines for equipment and practices[1] that can improve bariatric patient safety, comfort, and overall experiences in three parts of the perioperative setting.
PRE-OPERATIVE
The pre-operative experience sets the tone for a patient’s experience in your surgical facility. Position your high BMI patients for optimal outcomes the following ways:
- Evaluate and diversify waiting area seating. Waiting areas should include seating options for all patient body types, weights, and sizes. Offer standard-sized and wider chairs with generous weight thresholds as well as elevated chairs that ease sitting and standing for patients with skeletal muscular limitations.
- Consider your facility’s pre-operative assessment spaces. Most pre-operative patients are weighed, have vital signs taken, and change into gowns or other garments in a designated assessment space. Make sure this space offers ample room for movement and comfortable seating for patients of all sizes – key to alleviating anxiety before patients head into surgery.
TRANSFERS
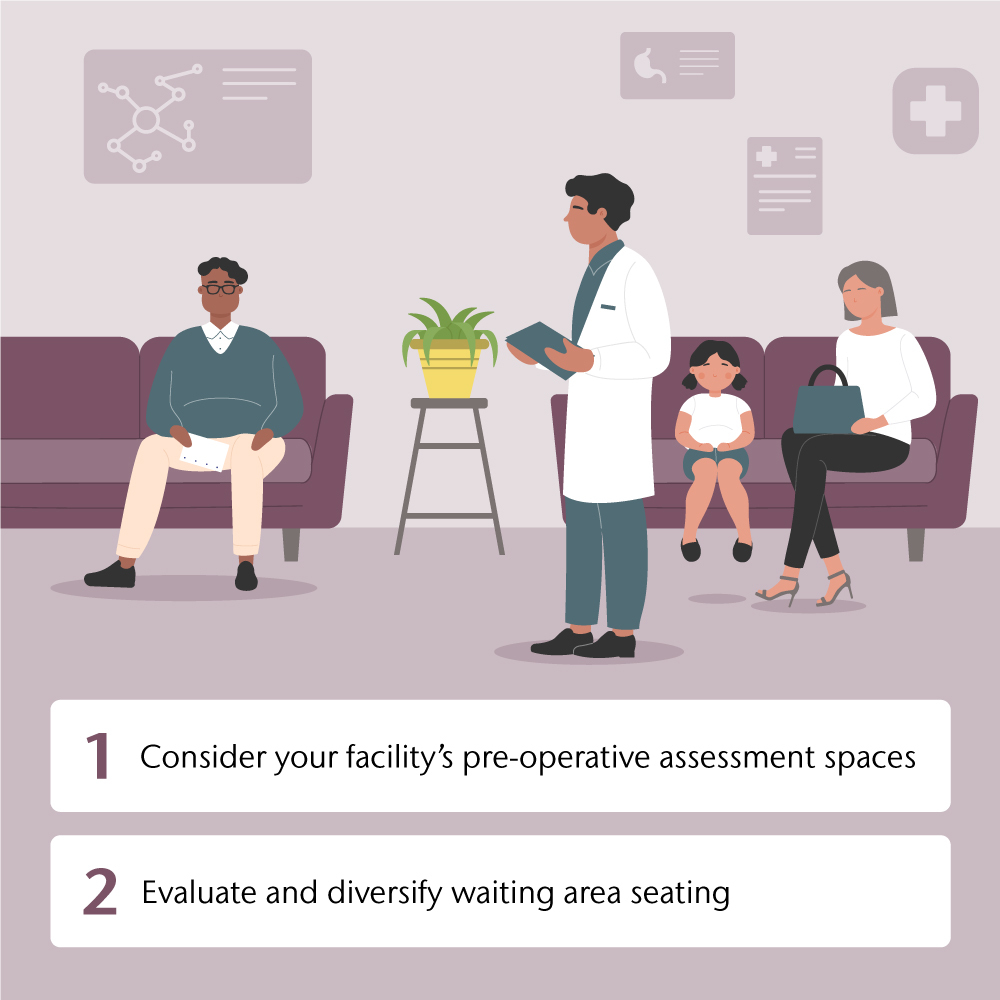
Keeping patients in alignment during transfers is crucial to reducing pain and risk of injury to both patients and caregivers. Of course, this requires added considerations and equipment for patients with high BMI:
- Stretchers. Motorized stretchers reduce necessary physical exertion on behalf of team members and are therefore very helpful for transferring bariatric patients.
- Wheelchairs. Surgical facilities should maintain wheelchairs in a variety of sizes.
- Transfer devices. Slide boards can present challenges when treating patients with higher BMI. Consider air-assisted transfer devices that have the added benefit of working in multiple settings. Breathable slings that can be left under patients also reduce risk and increase transfer control.
- Transport team size. A recurring topic across treatment of patients with high BMI is the matter of team size. Especially crucial during transfers, it also comes into play during repositioning and other common care scenarios (for example, when positioning bariatric patients’ legs in stirrups). Healthcare facilities are wise to establish clear guidelines that encourage care teams to enlist whatever number of professionals is needed to help with handling of bariatric patients.
- Hallways. Most facility hallways include turns, curves, and areas requiring badge entry. These necessitate stopping, starting, and the need for patient repositioning – all of which increase injury risk for high BMI patients especially. From keeping halls clear to reconsidering traffic patterns and even future building plans, assess opportunities to improve hallway transport in your setting.
- Hospital beds. Occasionally patients are taken from point A to point B on hospital beds, which can be difficult to steer and aren’t designed for transport – increasing injury risk for high BMI patients. If this or other equipment shortcuts and work-arounds happen frequently in your facility, consider – why? What can be done to ensure the availability of stretchers or other better-fit devices and equipment?
- Walking patients. If and when bariatric patients walk themselves to or from a surgical procedure, make sure they’re wearing non-slip foot protection. Have a plan and the appropriate equipment in place for lifting these patients in the event of a fall.
OPERATING ROOM
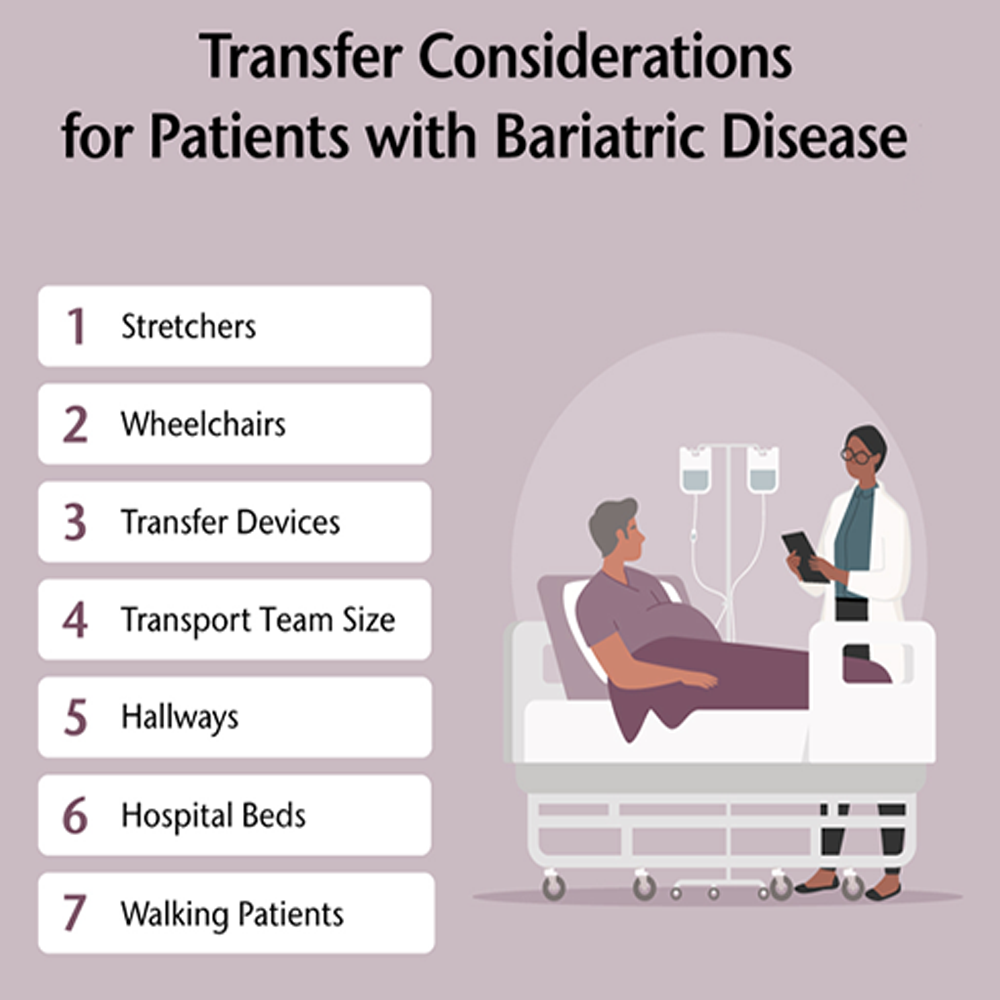
Most patients will be moved and positioned 7 to 10 times in the perioperative setting: Stretcher to operating table, potentially on and off of positioning devices, sliding up and down for anesthesia, and so on. Here are ways in which most operating rooms can improve bariatric patient safety in light of all of this movement:
- Display and abide by weight limits. Make sure weight limits as indicated in manufacturer’s instructions for use (IFU) are clearly labeled and displayed on beds, stretchers, wheelchairs, and other equipment. Remember, this extends to equipment like limb preppers and “candy cane” stirrups that clamp to beds and also have weight capacities.
- Reconsider draw sheets. If you take just one thing away from this piece, let it be this: hospital bed draw sheets should not be used for patient positioning in the OR. For all patients, but especially for patients with high BMI, draw sheets as repositioning aides dramatically increase risk of shearing and other skin injuries as well as other possible injuries for patients and caregivers. Plenty of alternatives to draw sheets exist; stock, train on, and utilize them!
- Consult Association of Perioperative Registered Nurses (AORN) recommendations. All of AORN’s guidelines, including its guidelines for safe patient handling and movement, can lead to smart decisions for care of patients with high BMI.
- Bed extenders. If you don’t have access to a bariatric operating room bed, consider bariatric width extenders. They attach to standard OR beds, taking the bed width from 20 inches to 28 inches.
This is just the beginning. Many more proven guidelines exist for positioning and caring for bariatric patients. Explore them and earn one free contact hour by listening to the full on-demand webinar.
[1] https://obesitymedicine.org/blog/shifting-from-morbid-obesity-to-class-iii-obesity/