4 Steps to Truly Effective Safe Patient Handling and Mobility (SPHM)
Earn one contact hour. Listen to the supplementary, free webinar on SPHM competency.
Dusting off your acute care setting’s SPHM practices is key to fewer injuries and stronger outcomes. Read on for helpful guidelines + listen to our on-demand webinar recording to earn one contact hour.
Most healthcare professionals have endured it: Training for equipment you know you’ll never use…or repeat training on equipment you know inside and out. Or maybe you “learned” how to use medical equipment at a skills fair, only to discover in a patient setting that you weren’t clear on it after all.
These are some of many gaps that get in the way of safe patient handling and mobility (SPHM) competency – loosely defined as a care provider’s ability to use SPHM equipment and follow associated policies and procedures with an actual patient in an actual patient environment on an ongoing basis. If staff isn’t competent and confident in SPHM devices and processes, SPHM goals are unlikely to be realized – a reality with risks for both patients and caregivers.
A complex topic? Yes. However, new and helpful rules of thumb are emerging.
Historically, checklists and annual mandatory training or skills fairs were used almost exclusively to assess SPHM competency. However, data shows these methods are largely ineffective, in part because they focus on technical skills while overlooking equally essential critical thinking and interpersonal skills. A renewed, more comprehensive approach to SPHM is at the heart of the Wright Competency Assessment Model.
The Wright Competency Assessment Model
Competencies can’t come from the top down and aren’t accomplished via checkboxes. These are key tenets of the increasingly popular Wright Competency Assessment Model.
Outlined in Donna Wright’s bestselling book, The Ultimate Guide to Competency Assessment in Health Care, the Wright Competency Assessment Model pushes past outdated and ineffective methods to help healthcare settings adopt an effective, efficient, and meaningful approach to SPHM programs, processes, and procedures. Here are four pillars of Wright’s framework:
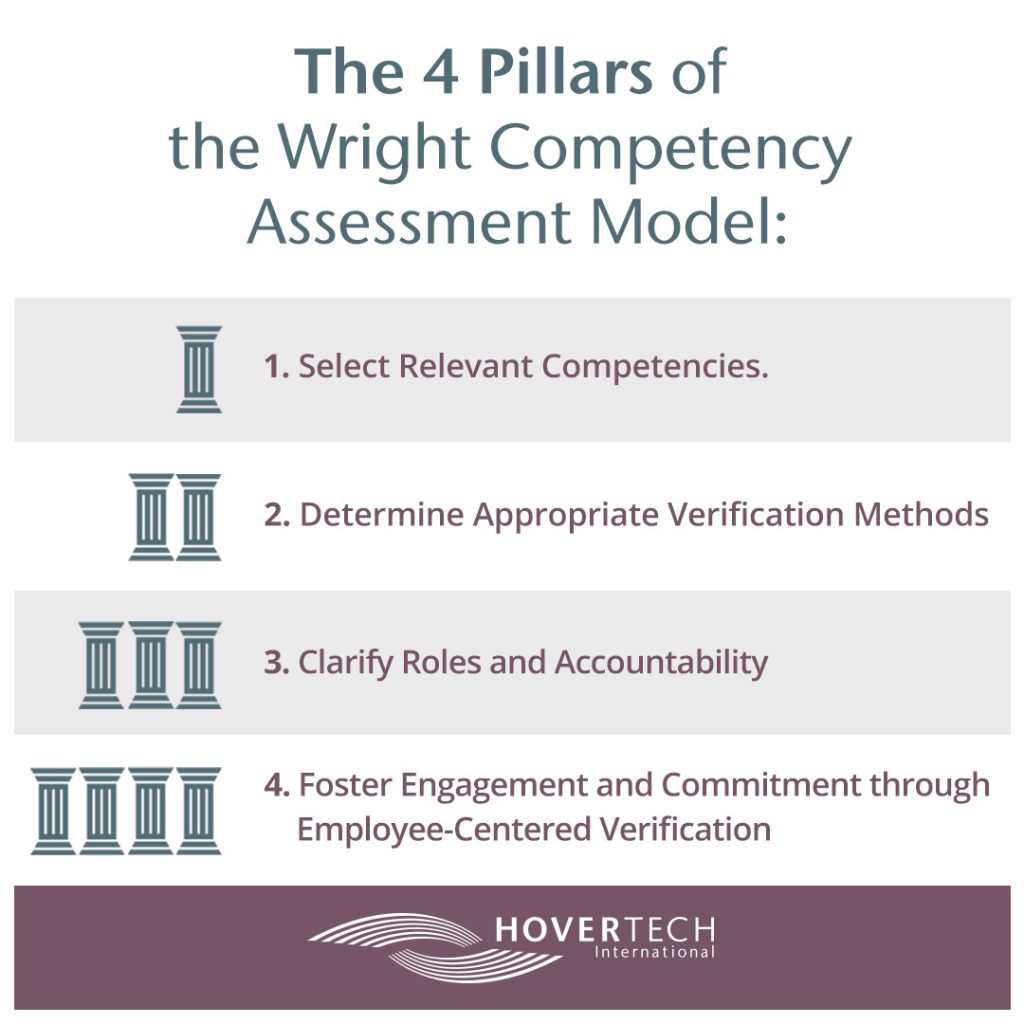
1. Select competencies that matter to the people involved and the organization.
It’s not uncommon for professionals to learn tasks they’ll never use. Meanwhile, there’s often no precedent for common real-world scenarios like lost supplies, malfunctioning equipment, or under-resourced care teams.
Closing these gaps requires competency training that is truly relevant to workplaces. It starts with competency selection.
A carefully selected list of highly-relevant competencies helps staff feel capable, engaged, and energized in their work. Conversely, a repetitive, everything-but-the-kitchen-sink list of competencies can be perceived as a disrespectful waste of time and can damage morale. By Wright’s standards, competencies should reflect reality, have ties to quality improvement data, and be chosen critically, through a dynamic and collaborative process. This is a far cry from checkbox-thinking or competencies chosen in a vacuum, without regard for what staff encounters in their day-to-day. It’s important to remember that competency selection usually is the responsibility of the organization. One of the biggest myths in healthcare is that mandatory competency training and milestones are dictated exclusively by external regulatory bodies. In reality, most competency determination is internal.
2. Select right-fit verification methods for each competency identified.
It’s one thing to demonstrate competency in a task. It’s another to demonstrate competency in the task in the face of pitfalls and challenges.
Take this story: A consultant performing SPHM analysis at a large teaching hospital saw two nurses lifting patients in side-by-side rooms. One nurse used a ceiling lift and a HoverSling® Repositioning Sheet. The other manually lifted the patient with a bedsheet, which exposes patients and caregivers to potential injury.
Both nurses had been trained in use of the ceiling lift and repositioning sheet. When the second nurse was asked why she didn’t use them, she responded that she couldn’t find the repositioning sheet – so she defaulted to the manual method.
Verification of SPHM methods has to go beyond the technical to the practical.This can require some outside-of-the-box thinking. One hospital unit coined the phrase “No Falls November.” Throughout the month, team members in banana costumes walked around asking nurses and CNAs questions related to safe patient handling – including questions about where items are stored and what to do in tricky or unforeseen circumstances. Correct answers earned yellow candy prizes! Unit managers in particular often see benefits from fun, real-time training that ensures staff is competent and that best practices are front and center in their minds.
3. Clarify the roles and accountability of the manager, educator, and employee in the competency process.
Professionals can’t be expected to approach a competency correctly – or at all – until they know that it’s expected and what is expected. Ensure that your workplace has a well-defined breakdown of responsibilities. Just as importantly, make sure there’s a no-fail system in place for communicating these responsibilities and related sub-responsibilities to each individual.
4. Employee-centered competency verification creates a culture of engagement and commitment.
Ownership, empowerment, and accountability are the three “legs” of the employee-centered competency verification “stool.” Ownership is established by identifying competencies that truly reflect the work. Empowerment comes when verification methods match the competency category. Last but not least, accountability is activated when well-considered checks and balances are put in place to ensure individuals can step into their competencies. In one scenario we encountered recently, a CNA knew how to move a patient from a bed to a recliner, but asked a director to handle it on her behalf. This skill is part of the CNA’s competency skills portfolio; she knew how to do it, but chose not to. Management subsequently addressed the matter. Commitment to accountability is as important as the competencies themselves in creating an engaged and responsive workplace.
Did you find this blog helpful? Send it to a fellow RN. Learn more about the Wright Competency Assessment Model and earn one contact hour by listening to a webinar led by Teresa Boynton, MS, OTR, CSPHP.
Want to learn more about the HoverSling® Repositioning Sheet and other patient handling and positioning tools? Contact HoverTech International.