Minimizing Pain, Maximizing Movement: SPHM for Severe Burn Patients
Listen to the Supplementary, Free Webinar on Moving Patients with Severe Burns
Nursing intervention for burns presents unique and high-stakes challenges. Read on for helpful guidelines and listen to the full on-demand webinar to earn one contact hour. Please note: Some photographs in the webinar and in this article might be considered graphic.
Almost half a million burn injuries occur in the United States each year. Approximately 10% require hospitalization. Once admitted, burn injury patients – like all patients – must be repositioned regularly as a key component of recovery and rehabilitation. This can prove daunting given the nature of burns and related treatment. In fact, burn nursing is emerging as a specialty nursing practice[1] – a testament to the complexity of this line of care.
Below, we offer guidelines for safe patient handling and mobility (SPHM) for victims of severe burns – guidelines that can advance the goal of restoring a patient’s pre-injury baseline range of movement.
First, a refresher on the value of patient movement.
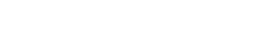
HOW MOVEMENT HELPS
Burn patients need to be repositioned, turned, and moved for the same reasons all patients need to be moved, and a few more:
- Movement offsets the effects of prolonged bedrest. It can restore blood flow and help preserve unburned skin tissue. This is key to preventing pressure injuries.
- Movement strengthens pulmonary function (including regional ventilation in the lungs) and helps range of motion and muscle strength. It can keep urinary stasis at bay by encouraging bladder drainage, and also facilitates mucus drainage.
- Movement can improve a patient’s mental status, offering a new visual perspective and opportunity for caretaker engagement.
- For burn patients in particular, movement is part and parcel of physical and occupational therapy that’s essential to larger rehabilitation.
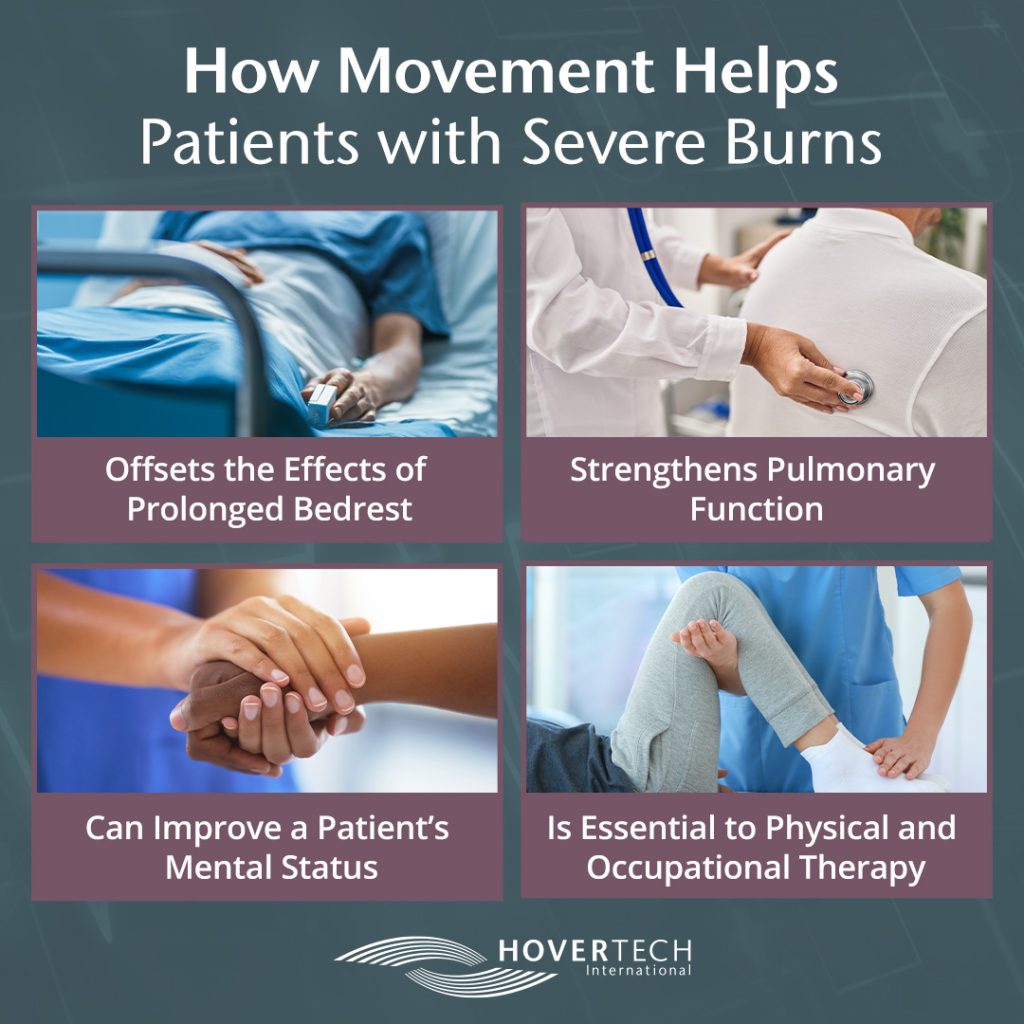
PATIENT MOVEMENT IN PRACTICE
General safe patient handling and mobility best practices apply to patients who have incurred severe burns:
- Nurses and therapists should maintain good alignment and be as close to the patient as possible when repositioning.
- Set the bed at proper height.
- Use a lift pad or sheet.
- Consider lifts and slings for dressing limbs.
- A waist belt or a lift can be helpful when lifting the patient or moving them into a seated position.
- Enlist fellow staff whenever needed.
The unique challenge with burn patients, of course, is the high degree of modification required to accommodate sensitive burned or grafted areas and donor sites, as well as limitations imposed by dressings and equipment. Grafted sites and related splints are particularly limiting. Surgical teams typically request 5 to 7 days for grafts to adhere before range of motion is performed. When possible, maximize joint movement before a patient undergoes skin grafting to help offset the effects of restricted movement in the days ahead.
Some overarching considerations for safe handling of burn patients:
- During and beyond standard repositioning (which is performed every two hours or less), place a high degree of attention on joint movement, as joints are critical to restoration of baseline function. Even tiny micro-movements (having patients flex fingers, or repositioning their limbs ever so slightly while they’re sleeping) can be beneficial.
- As soon as physically possible, position patients sitting up in bed at a 30-degree angle – key to pulmonary health. Pillows can help prevent sliding. Piling two to three pillows can also be helpful for turning patients onto their side, and holding the position. Add absorbent mats to pillows when patients are experiencing skin sloughing.
- Engage with patients during repositioning. This lets them anticipate the movement and can also boost mental status. Patients recovering from burns are often reticent to move; remind them that movement is essential to recovery.
- As patients progress to sitting up and as they become ambulatory, be on alert for orthostatic hypotension. Prevent against it by monitoring blood pressure and repeatedly asking patients how they feel.
- In time, a patient might begin to regain the ability and desire to move. Let them assist you with movements as they’re able. With therapists’ approval, instruct patients on how to bend a knee, use a bedpan, and other functions medical staff might have grown accustomed to performing on their behalf.
- Splints over grafted joint extremities like elbow and knees are designed to keep them from bending as grafts adhere. Caregivers might be tempted to leave the splinted limb alone; however, it’s wise to move the entire splinted limb when possible. Once splints are removed, you can begin to bend joints – gently at first, building up to increased movement.
- Dressing changes are often ideal times to perform range of motion exercises, as bandages and other obstructions are temporarily removed. Work with therapy teams to take advantage of this timing. Strive to medicate patients 15 to 20 minutes before these sessions for higher tolerance, which usually translates to greater progress.
PRE-AMBULATORY MOVEMENT
Dangling a patient’s legs over the bed has circulatory, pulmonary, and gastrointestinal benefits, and can offer patients a sense of accomplishment. A waist belt can ease the process of moving a patient safely into this position (remember, you might need to adjust the belt to avoid burned areas, moving it up or down by a few inches as needed). Occupational and physical therapists can help you determine the length of time your patient can tolerate leg dangling.
BECOMING AMBULATORY
Once a patient can stand – assisted or unassisted – the care team might explore the possibility of assisted walking. Ambulating has gastrointestinal and pulmonary benefits. Like all movement, it can also boost a patient’s outlook. Thoracic walkers are valuable to early ambulating among burn patients, as they can accommodate oxygen tanks and drainage bags. Even more, thoracic walkers’ seat pads allow patients to sit and take a break as needed.
Strengthening and range of motion exercises layered atop standard repositioning offers burn patients the highest chances of significant or complete return to baseline movement.
Did you find this blog helpful? Send it to a fellow RN. For more nursing education on SPHM for severe burns, and to earn one free contact hour, listen to the full on-demand webinar.
For more information on safe patient handling tools that help prevent pressure injuries, contact HoverTech International.
[1] https://www.nursingworld.org/news/news-releases/2020/ana-recognizes-burn-nursing-as-new-specialty-nursing-practice/