How the ABCDEF Liberation Bundle Shortens ICU Stays at Northwell Health
Each year, there are four million intensive care unit (ICU) admissions in the United States. Here’s how one leading healthcare system is using the ABCDEF Liberation Bundle to reduce ICU length of stay and related spending. Listen to the full on-demand webinar to earn one contact hour.
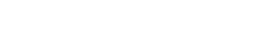
Nearly 27 percent of hospital stays involve ICU services which cost, on average, 2.5 times more than their non-ICU counterparts.
The prospect of shortening ICU stays is a medically and operationally complex and sensitive matter. Still, some healthcare systems are making headway, aligning people, processes, and technology to safely reduce ICU length of stay when it makes clinical sense. New York’s Northwell Health is among them. Their guiding tool? The Adult ICU Liberation Bundle.
ABCDEF LIBERATION BUNDLE EXPLAINED
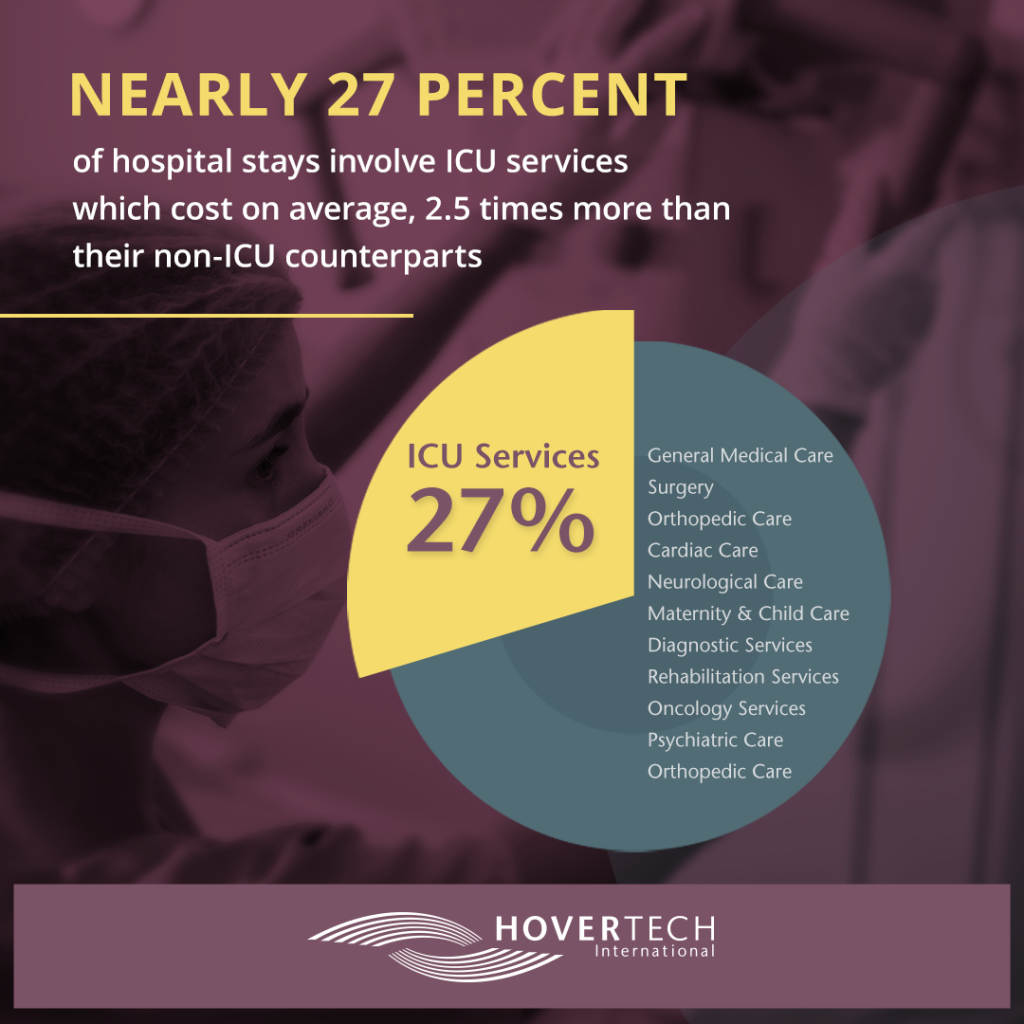
Developed by the Society of Critical Care Medicine in 2014, the Adult ICU Liberation Bundle, also known as the ABCDEF Bundle, is a set of evidence-based guidelines designed to help healthcare settings activate organizational changes that can get patients out of the ICU sooner, largely by avoiding unnecessary sedation and comas.
ABCDEF is an acrostic for remembering six key steps:
- Analgesia: Assess, Prevent, and Manage Pain
- Both Spontaneous Awakening Trials and Spontaneous Breathing Trials
- Choice of Analgesia and Sedation
- Delirium Identification and Management
- Early Exercise and Mobility
- Family Engagement and Empowerment
(Of note: F – family engagement and empowerment – was added in 2023.)
Northwell Health, tri-state New York’s largest healthcare system with 18 hospitals, began implementing ABCDEF guidelines in its critical care units in 2014.
Beyond benefits for process, care coordination, and communication, both ICU length of stay and ventilator duration at Northwell Health have declined, and continue to decline, in the decade since the program was launched.
Here, we’ll outline some key components of Northwell Health’s ABCDEF Liberation Bundle success.
SETTING THE STAGE FOR CHANGE
Foresight, planning, and expectation-setting were the first steps toward favorable ABCDEF results at Northwell Health.
Before adopting the program in 2014, Northwell Health decided to track and measure each stage of the process using the PDSA Methodology for Continuous Improvement:
- Plan (development by clinical teams of a plan based on needs assessment)
- Do (plan execution)
- Study (collect data and review performance indicators)
- Act (use study data to adjust, adopt, or abandon plans accordingly)
Data is continually collected across the healthcare system’s 500+ critical care beds via Apache Spark, a large-scale data analytics tool. Length of ICU stay and number of ventilator days in multiple ICUs (including specialty ICU units like cardiac thoracic, trauma, and burn) are tracked by clinicians. Results are displayed via metrics and dashboards custom-built into Northwell Health’s electronic medical record system, or EMR. Front line leaders also have access to a tool that assesses, in real time, patients in their unit. The sum total of all of this is easy tracking of variables and outcomes.
SPONTANEOUS AWAKENING AND BREATHING TRIALS
Moving onto the benefits of ABCDEF Liberation Bundle itself:
While all aspects of ABCDEF are valuable, Northwell Health can’t overstate the value of letter B: Both Spontaneous Awakening Trials (SAT) and Spontaneous Breathing Trials (SBT). SAT and SBT proactively determine whether ICU patients can be safely weaned off of sedation and mechanical breathing which, when successful, can lead to decreased length of ICU stay. Today, every Northwell Health critical care patient is assessed for SAT eligibility. Assessment is conducted via the Richmond Agitation Sedation Scale (RASS), which gauges consciousness; the Confusion Assessment Method (CAM) Delirium for ICU, which determine delirium levels; and discussions with physicians to discuss contraindications and other considerations.
In eligible patients, sedating medications are strategically decreased. If a patient moves outside of the acceptable range of sedation during the trial, medication is restored. If a patient remains alert, appropriate, and within an acceptable consciousness range, discussions begin withrespiratory therapists about the second part of B: eligibility for a spontaneous breathing trial. SBTs are performed on eligible patients under careful watch of a respiratory therapist who measures respiratory mechanics in accordance with guidelines and criteria as a patient is weaned off of mechanical ventilation assistance. In successful scenarios, patients proceed to extubation – bringing them one step closer to possible ICU discharge.
EARLY EXERCISE AND MOBILITY
Early mobilization of ICU patients is another key component of Northwell Health’s ABCDEF success. This comes as no surprise to researchers. Studies continually show that mobility and exercise can contribute to successful ICU awakening and extubation and earlier functional recovery overall. Even the simplest interventions like patient turning and better posture aide a patient’s recovery (many ICU patients can achieve mobility milestones like rolling in bed, sitting at edge of bed, sitting, even standing and walking). Research has shown minimal (and often no) adverse events happen in early ICU mobilization – and none associated with death. In short, the benefits of patient mobility in ICU clearly outweigh the risks. And just because an ICU patient might appear unable to mobilize doesn’t necessarily mean they shouldn’t or can’t.
Of course, mobilizing critical care patient does involve qualifications, caveats, and nuance that can intimidate some clinicians. This reality drives organization-wide messaging constantly reinforced at Northwell Health: That no matter a patient’s mobility level, it is everyone’s responsibility to promote and participate in it. All ICU clinicians should undergo proper training, exercise proper assessments, and use clinical judgment to determine if and how patients are safe to mobilize.
To prevent delays and create culture change at Northwell Health, order sets were created in EMR to promote the early exercise and mobility component of the ABCDEF bundle. Today, activity is almost always the norm for patients unless otherwise contraindicated.
The following can help set the stage for more safe patient mobility in the ICU:
Safe patient handling and mobility equipment.
Use of safe patient mobility equipment is mandated by New York State’s Safe Patient Handling Law and is a system-wide standard at Northwell Health. Mechanical lifts or ceiling lifts can help get patients from a bed to chair, and vice versa.
Plan ahead for lines and tubes.
Common in the ICU, lines and tubes can challenge mobilization – but should not be a deterrent. Growing evidence shows patients on endotracheal intubation (ETT), extracorporeal membrane oxygenation (ECMO), and continuous renal replacement therapy (CRRT) can be safely mobilized as long as a mobility plan is coordinated and communicated to clinicians involved in the patient’scare. Ask fellow clinicians to help you move lines and tubes to allow for patient movement.
Use outcome measures.
Adoption of outcome measures can help care teams determine patients’ functional capacity, track progress, set achievable goals, put a patient on a path to functional recovery, and communicate with one another more clearly and consistently thanks to outcome measurement system vernacular. Below are some of the measuring tools used at Northwell Health; all are simple, easy to use, and transferrable across disciplines:
- AM-PAC “6 Clicks”
- John Hopkins Highest Level of Mobility (JH-HLM) scale
- 6-Minute Walk Test
- Modified Borg Rate of Perceived Exertion (RPE) scale
- Physical Function in Intensive Care (PFITS) test
In sum, Northwell Health’s adoption of the Society of Critical Care Medicine’s ABCDEF bundle and related best practices has successfully decreased the healthcare system’s ICU length of stay, ventilator days, and use of sedation. At the same time, it has educated the healthcare system’s frontline staff on the importance of early mobility in critical care.
For a more in-depth talk and to earn one free contact hour, listen to the full on-demand webinar.