The Importance of BMAT and Other Assessments to SPHM – and How to Make EHR Assessments More Nurse‑Friendly
Effective use of safe patient handling and mobility (SPHM) equipment starts by properly assessing patient mobility. Discover ideas for formatting electronic health records (EHR) assessments for easier and stronger data entry via fewer clicks and screens. Listen to the full on-demand webinar to earn one contact hour.
Accurate, comprehensive electronic health record (EHR) data entry is critical to patient care. In today’s fast-paced medical landscape, though, data entry is often compromised. Sometimes clinicians let an EHR checklist, rather than a patient’s actual status, guide documentation, skewing accuracy. Other times no observations or insights are entered into open-ended form fields. There’s even occasional failure to indicate change in a patient’s condition – dire in any situation, but especially when a patient has declined.
These lapses and oversights impede the standardization of evidence-based care, which is essential to the goal of consistently doing the right thing for every patient, every time. They also jeopardize many aspects of patient care plan, including safe patient handling and mobility (SPHM). After all, choosing the best SPHM equipment starts by understanding a patient’s real-time mobility status and needs.
But such lapses can harm nurses, too: According to the 2020 Nurses Malpractice Claim report, treatment and care-related allegations continue to represent the highest percentage of all malpractice claims asserted against nurses. Many of these allegations tie back to documentation deficiencies and can result in professional liability lawsuits or even action against a nurse’s license.
Below, we’ll outline ways to improve EHR usability in efforts to make assessment-related data entry more intuitive and efficient for nurses and other practitioners. But first, a reminder how we got here.
DOCUMENTING IN THE AGE OF EHR
Rapid adoption of EHR (also known as electronic medical records, or EMR) followed passage of the Health Information Technology for Economic and Clinical Health (HITECH) Act in 2009.
While HITECH has improved many aspects of healthcare quality, patient safety, and diagnostic accuracy, it has also ushered in unintended consequences, most stemming from increases in documentation time involved in digital record-keeping. By some accounts, physicians today spent twice as much time on electronic documentation and clerical tasks as they do providing direct patient care. Nurses have also been shown to devote more than half of their clinical hours to EHR data entry and retrieval, and also report diminished patient contact.
Known as the documentation burden, the widespread discontent stemming from time-intensive EHR-related administration has been linked to increases in medical errors, threats to patient safety, job attrition, even burnout among nurses and physicians. Some physicians have even reported a willingness to be out of compliance with EHR incentive programs in favor of mitigating the documentation burden.
Consequently, there are pushes to reduce EHR-related clinician burdens. In March of 2020 the Department of Health and Human Services stated three goals: to reduce time and effort required to document health information, reduce the effort needed to meet regulatory requirements, and to improve EHR ease of use overall. The Nursing Knowledge Big Data Science (NKBDS) Initiative has committed to better standardization and integration of the information nurses gather in EHRs. Their priorities include increased interoperability, or the ability of different EHR systems to “access, exchange, integrate and cooperatively use data” across organizations and boundaries – key to weaving assessment results into patient’s larger care plan, and a topic we’ll elaborate on below.
THE IMPACT OF EHR ON SPHM
Which brings us back to SPHM. From air-assisted devices to slings and lifts, an abundance of technology has been developed in recent years to alleviate patient handling and mobility barriers. These technologies reflect evidence-based data showing that early, frequent patient mobilization often leads to better patient outcomes, as it allows for several key aspects of care:
- Safer testing (such as use of a stand-to-lift if orthostatic hypotension is suspected, or if an orthostatic hypotension screening is positive)
- Completion of care tasks (such as easier boosting of a patient in bed without risk of friction and shear)
- Easier strengthening and progress (such as ambulating in a hallway to increase endurance and step count while also minimizing risk of falls)
Often the same SPHM device is used for more than one of these purposes; for example, a powered sit-to-stand device might allow for a bed-to-toilet transfer at night and, later, help a patient get upright so they can strengthen by marching in place.
Of course, choosing the right SPHM equipment for a patient and incorporating it into their care depends heavily on the accuracy of patient mobility assessments as entered into the EHR. This puts the onus on nurses and other practitioners to accurately and comprehensively enter EHR assessments, which can be aided by EHR design that’s more user-friendly.
INCORPORATING COMMON ASSESSMENT TOOLS INTO EHR
The Bedside Mobility Assessment Tool (BMAT) and the Dionne’s Egress Test (EDT) are the most frequently used mobility screening and assessment tools in U.S. hospitals; a variety of additional fall risk screening tools are also readily utilized. All too often, though, these assessments as implemented in EHR are difficult to read and navigate, don’t mirror practitioner logic, or offer other practical hurdles.
The good news: Major EHR software brands are fairly – if not highly – customizable. Hospital leadership and chromatic specialists can and should have a say in how assessments flow and appear within EHR design. Many hospitals self-build their EHRs with strong input from clinical leadership in order to best meet the needs of frontline staff.
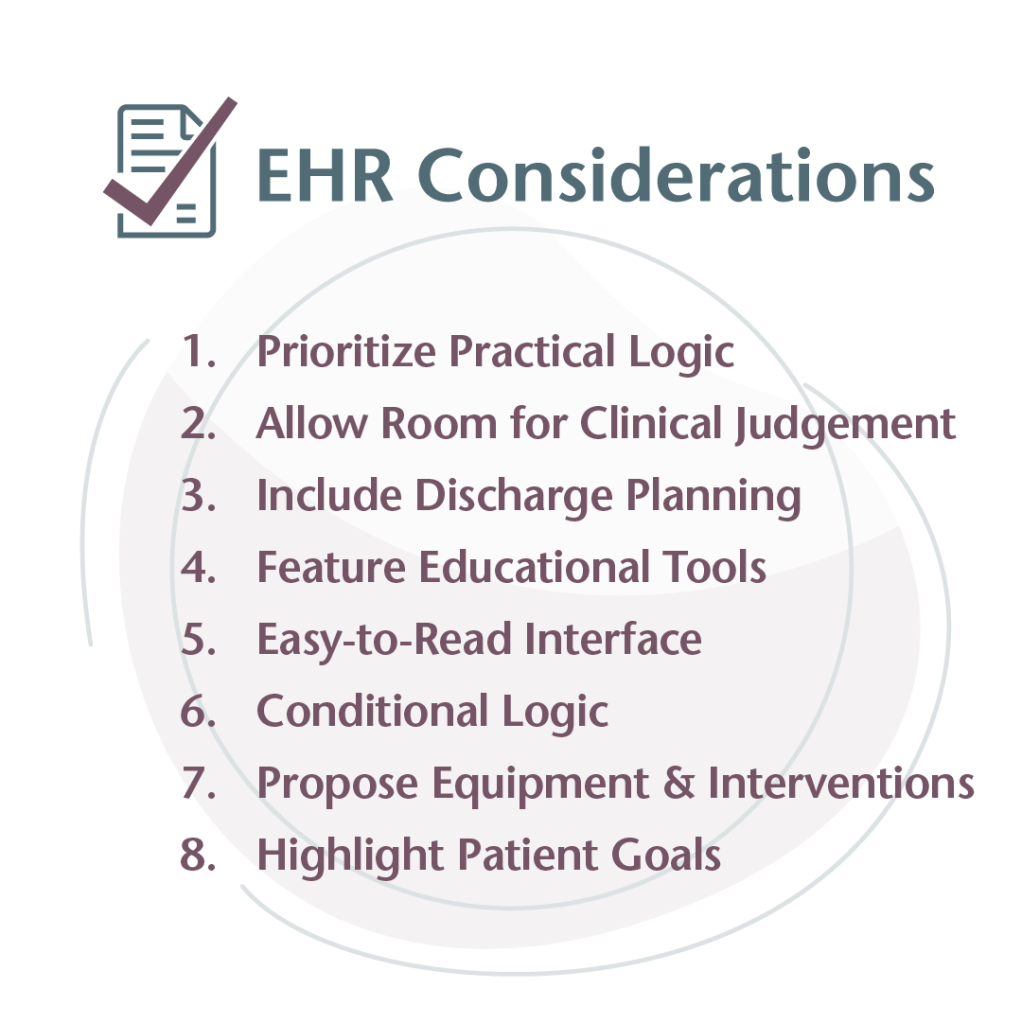
What do well-integrated assessments look like? Below are examples of mobility and fall risk assessments built into EHR in a manner worth noting and considering. Decision-makers can use these examples to inform how their own assessment tools are designed and woven into the larger EHR to ensure interoperability, ease of use, and optimal data entry – key to setting the stage for consistent, effective use of SPHM equipment.
EHR CONSIDERATION #1: PRIORITIZE PRACTICAL LOGIC

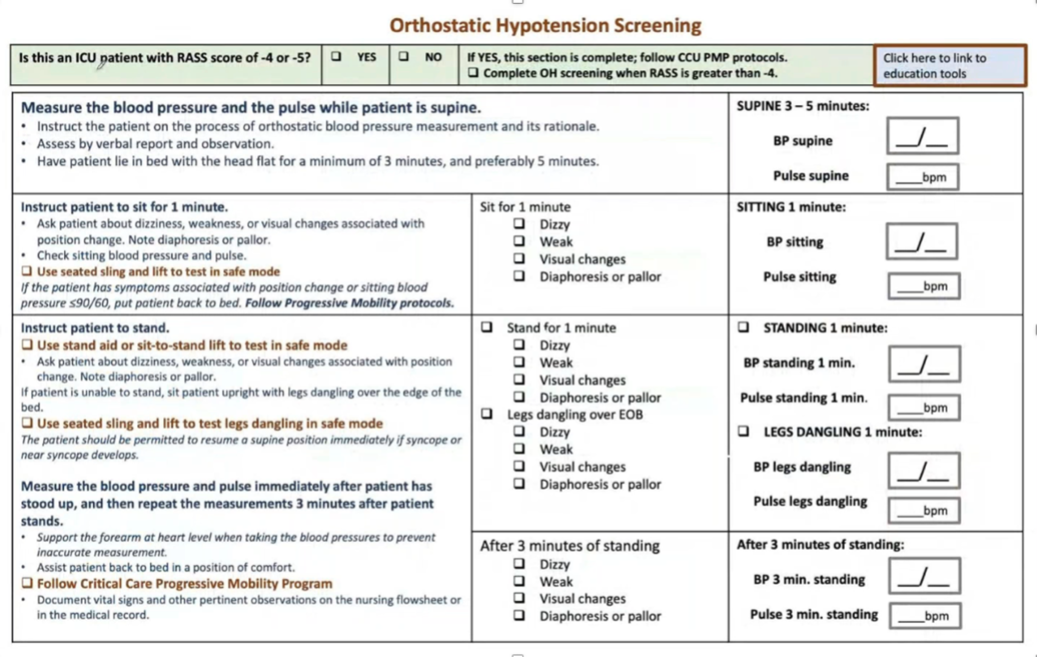
The screen shot above shows the Morse Fall Scale assessment as built into a Cerner EHR in 2013. Note the question at the top: “Is this an ICU patient with a RASS [Richmond Agitation Sedation Scale] score of -4 or -5?”
In this assessment’s early years, this question was not included – a void that created angst among ICU nurses treating deeply sedated or unarousable patients ineligible for the fall scale assessment. The nurses had no choice but to complete the assessment on behalf of these patients in order to continue on with data entry. Falsifying answers in the interest of progressing in EHR comes with the risk of potential license and professional liability issues; however, in the moment, nurses had no choice. To err on the side of safety, most indicated that patients were high fall risk even when that wasn’t the case.
Eventually, to fix the problem, this key determining question – “Is this an ICU patient with a RASS [Richmond Agitation Sedation Scale] score of -4 or -5?” – was added, allowing nurses of deeply sedated and unarousable patients to bypass the non-applicable question and move on. This example highlights the importance of asking: Is an assessment an accurate reflection of all possible clinical realities a nurse might face while responding? Or are clinicians being forced to answer prompts and questions that might not apply to the patients in their care at this time? Do they need to return to the assessment and complete it when appropriate?
EHR CONSIDERATION #2: ALLOW ROOM FOR CLINICAL JUDGMENT

The image above shows the remainder of the Morse Fall Scale assessment within the same Cerner EHR build.
This screen includes elements added at the request of the ICU nurses who utilize the program, including the addition circled on the right, which lets practitioners deem a patient a high fall risk even if they’d scored below 44 on the Morse Fall Scale (a score below 44 theoretically indicates a patient is not at high risk for falling). This addition stemmed from nurses vocalizing their belief that their own clinical judgment, when necessary, should be allowed to supersede an assessment score within the EHR. It highlights yet another key consideration when designing EHR content: When it makes sense, allow clinicians the choice of infusing their expertise so that important patient assessment conclusions and interventions aren’t drawn from scores or algorithms alone.
EHR CONSIDERATION #3: INCLUDE DISCHARGE PLANNING
Health practitioners talk a lot about the value of discharge planning, and how it should start on at admission – but usually lack a system for documenting and tracking progress accordingly.
At the bottom of the screen above there is a discharge planning checklist featuring a free text box that lets practitioners add checklist items as they see fit. This particular hospital also created a digital interactive tool to engage patients and caregivers in discharge preparation; it helps ensure that checklist items are understood and carried out once a patient returns home. This particular EHR checklist might benefit from the addition of statements requiring agreements from patient and their families – statements like, “I understand what I can do to prevent falls” and, “I understand how to use my assisted device for safe walking.”
EHR CONSIDERATION #4: FEATURE EDUCATIONAL TOOLS
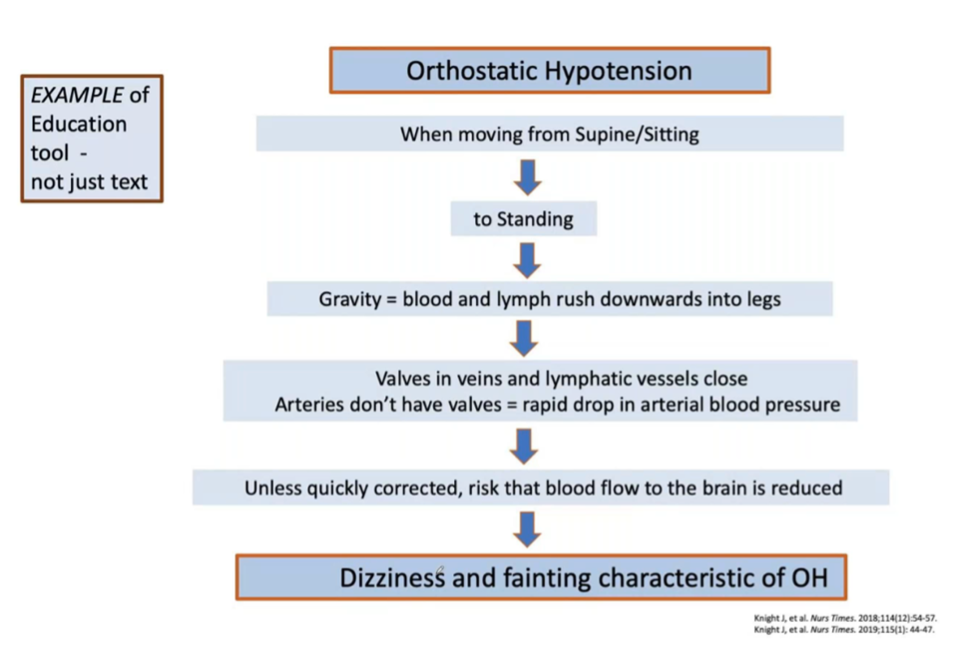
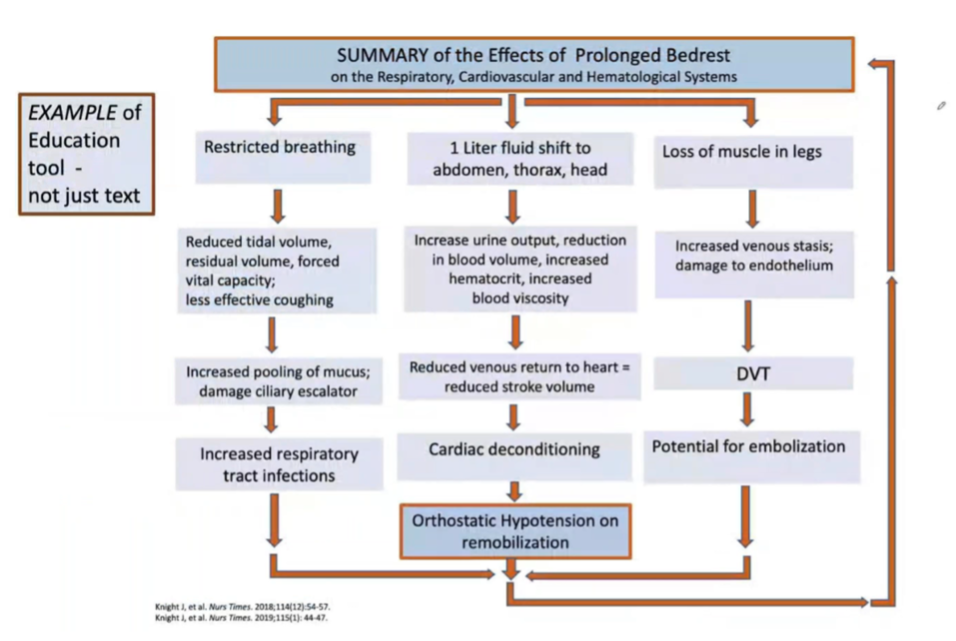
The charts above are examples of educational screens that can also be integrated into the EHR to refresh or inform clinicians’ understanding of topics likely to pertain to the patient at hand. Ask yourself: What information might be helpful to a nurse at this particular patient juncture? Consider flowcharts like these as well as other graph types and illustrations to efficiently and effectively offer information that will aide clinical practice versus only using text or articles.
EHR CONSIDERATION #5: EASY-TO-READ INTERFACE
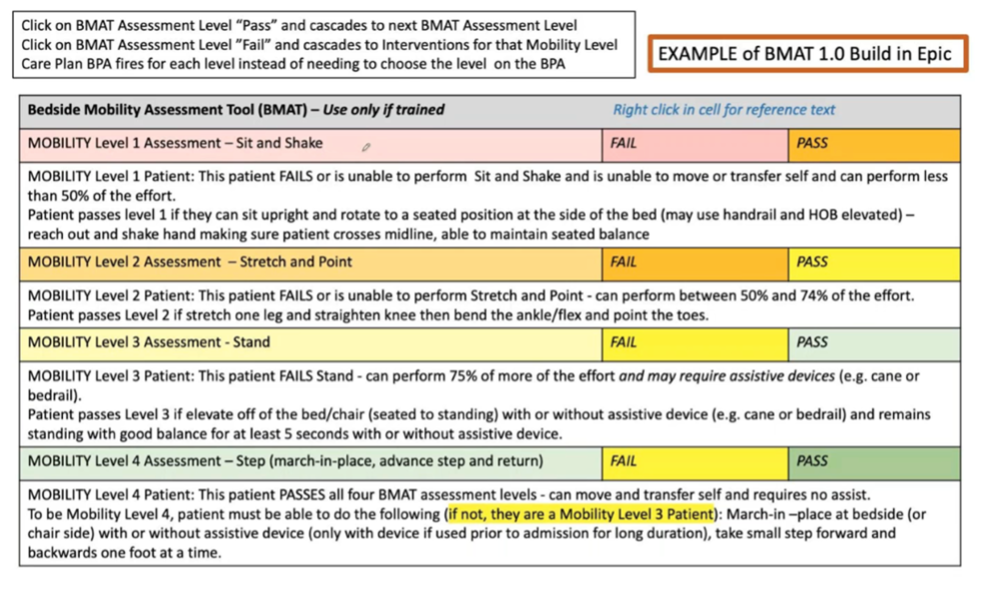
Easy readability within interface design is integral to the EHR experience and subsequent patient outcomes. Professional developers should prioritize design that’s streamlined, not too busy, and all in all digestible. However, it’s nonetheless wise for hospital teams to keep an eye on this critical design factor, as well, to ensure that readability doesn’t lose out to other considerations.
The screen above is an example of a presentation that’s well organized, easy on the eyes, and that uses color (different mobility assessment levels are assigned to different shades) to improve ease of reading.
EHR CONSIDERATION #6: CONDITIONAL LOGIC
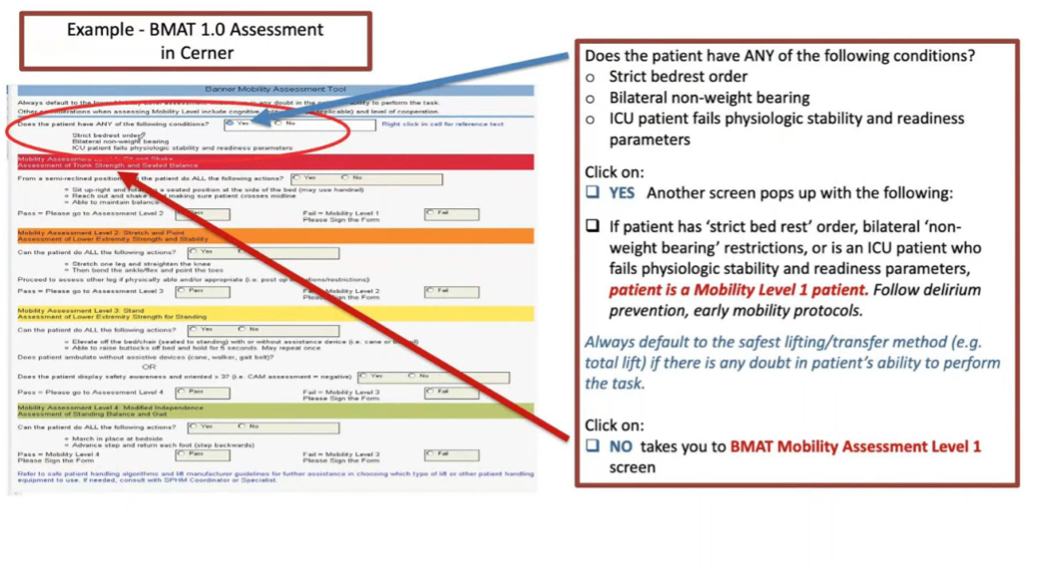
Conditional logic indicates a user journey that’s dependent on how a user responds (click yes and move to one screen, click no and move to another, for example). Conditional logic is typically the mark of a truly intuitive and comprehensive EHR assessment, as it can readily accommodate a wide variety of clinical realities and doesn’t default to “one size fits all” messaging.
The screen above shows conditional logic in action. As is explained in the margin box, users journey on to one of two very different screens based on their response to the question, “Does the patient have ANY of the following conditions?”
EHR CONSIDERATION #7: PROPOSE EQUIPMENT AND INTERVENTIONS
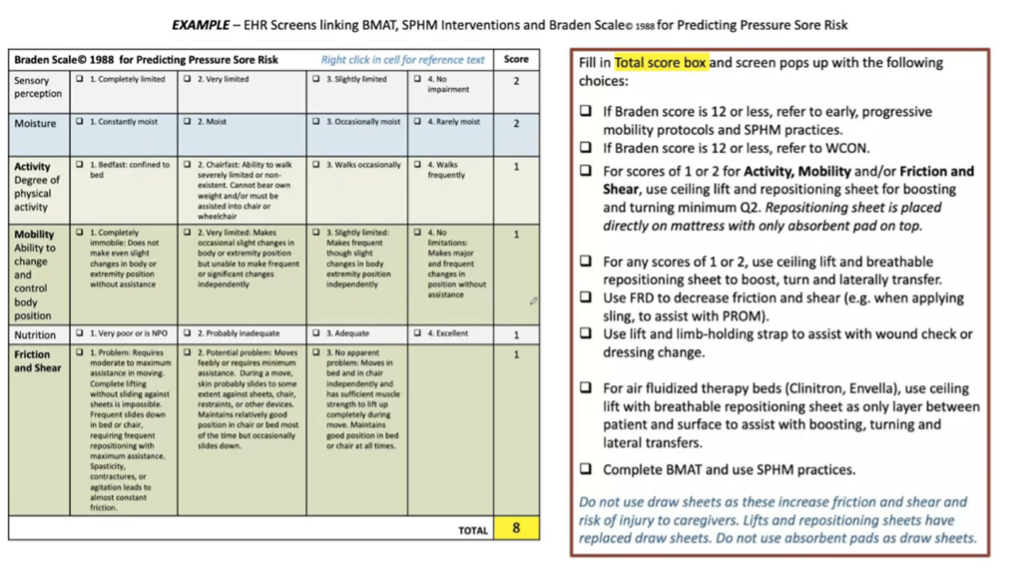
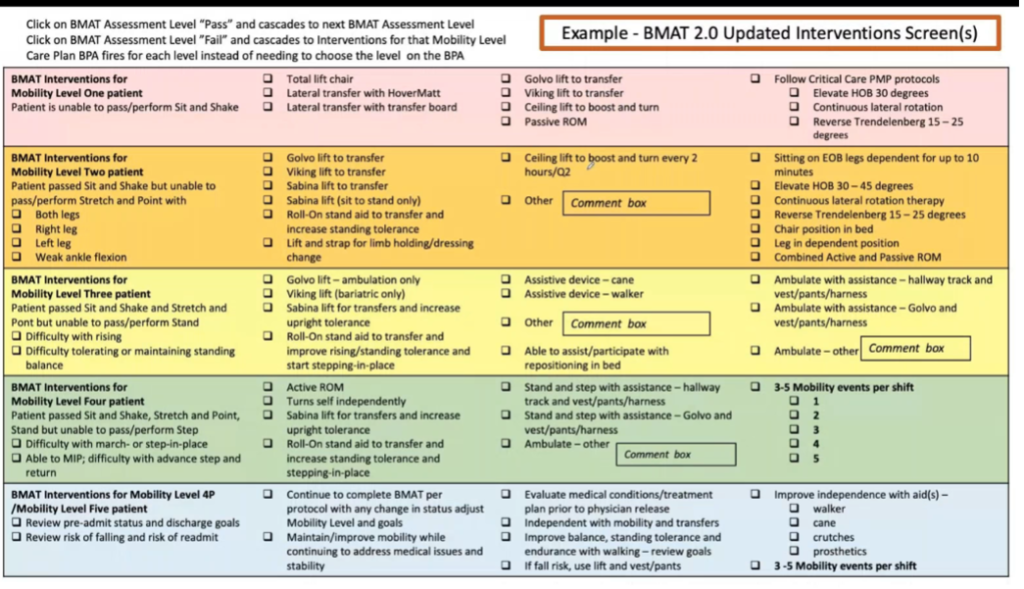
There’s no reason EHR assessments can’t include recommendations for specific SPHM equipment and interventions, as shown in the three screens above.
The third of these screens was designed for and used by a hospital with a stated focus on mobility events per shift. This is how they ultimately decided to ensure nurses understand and document interventions based on a patient’s exact BMAT classification. It’s also another great example of color coding in action.
EHR CONSIDERATION #8: HIGHLIGHT PATIENT GOALS
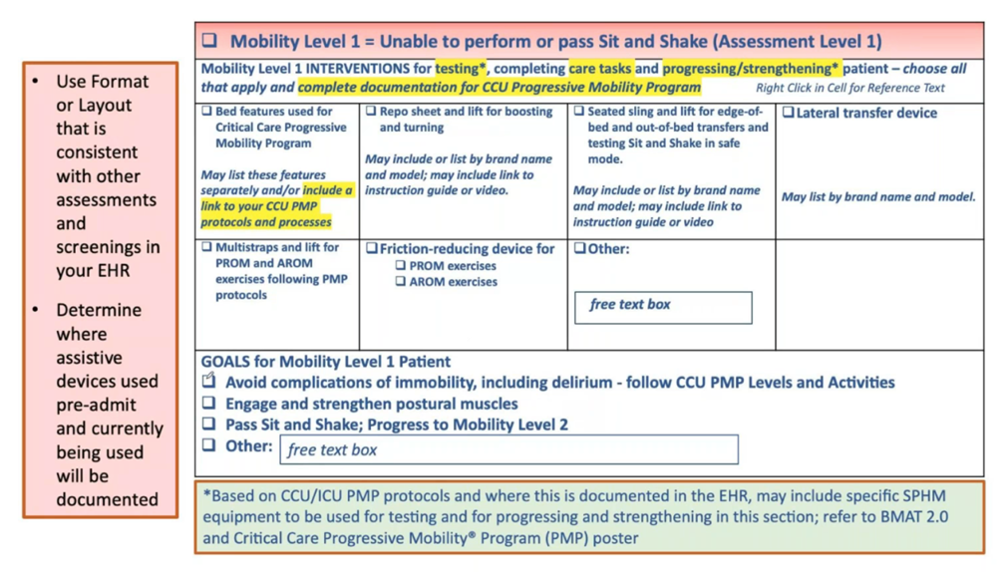
In dynamic clinical settings, it can be easy to lose sight of a patient’s individualized goals – or perhaps even know what they are in the first place. The bottom of the screen above shows an instance of a hospital ensuring that nurses see a patient’s specific mobility goals within the EHR – key to making sure recommended interventions and steps are taken.
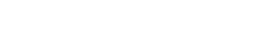
In conclusion, when considering the integration of assessments into electronic health records, ask yourself:
What aspects of mobility and fall assessment need to be considered and documented in order for staff to make the right choices related to SPHM equipment?
Weight bearing status, patient motivation and cooperation, cognitive and delirium assessments, and early progressive mobility activities are just a few matters that might be relevant. When embarking on an EHR build or redesign, make sure all of these are included, and, better yet, are linked to related resources: device recommendations, fall risk assessments, orthostatic hypertension assessments, and skin assessment and grading, to name a few. Again, your EHR software provider should be able to help you implement the most effective and user-friendly EHR system, methods, and design based not only on their expertise, but on what is working for other hospitals and healthcare organizations they serve.
Want to see more examples of BMAT and other mobility assessments built into electronic health records? Learn more and earn one free contact hour by listening to the full on-demand webinar.
Teresa Boynton, MS, OTR, CSPHP

Currently an independent consultant, from 2015 to 2018 Teresa Boynton, MS, OTR, CSPHP worked for Hill-Rom, assisting healthcare facilities in building safe patient handling and mobility (SPMH) programs. Prior, Teresa worked for Banner Health for 26+ years where she focused on preventing caregiver injuries, resolving workers’ compensation claims, and implementing a standardized SPHM and fall prevention program. In 2003 she began work on what became the Bedside Mobility Assessment Tool (BMAT). She and nurse colleagues developed BMAT 2.0 and published an article and support tools in the July 2020 issue of American Nurse Journal. Teresa received a 2020 Innovation Award from the National Board for Certification in Occupational Therapy for her work on developing and implementing BMAT and related SPHM programs. She is a longtime member of the Association of Safe Patient Handling Professionals (ASPHP). In 2000, Teresa took a sabbatical and worked as a paralegal for a medical malpractice defense attorney where she gained a greater appreciation for standardized practice and accurate documentation – an experience that informs and energizes her work to this day.